What is TMJ, anyway?
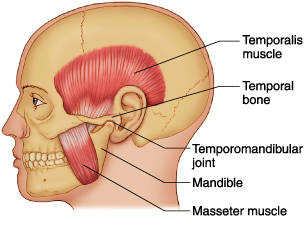 “TMJ” stands for temporomandibular joint. These joints, (one in front of each ear), are what allow the jaw to hinge open and closed when chewing, yawning, and talking. The acronyms TMJD or TMD may be used to describe a dysfunction of the joint, disc, or other tissues in the area of the jaw.
“TMJ” stands for temporomandibular joint. These joints, (one in front of each ear), are what allow the jaw to hinge open and closed when chewing, yawning, and talking. The acronyms TMJD or TMD may be used to describe a dysfunction of the joint, disc, or other tissues in the area of the jaw.
Why does my Massage Therapist want to know if I have jaw pain? And what can they do about it?
Jaw pain and dysfunction can be related to other issues that your massage therapist is addressing, and they may be able to help improve both by also treating the tissues surrounding the TMJs.
In particular, pain referral between the TMJ structures and headache are common, with either being the primary issue. The tissues in these areas are closely linked, and “the pain referral is primarily related to the overlap of anatomy and neural innervations” (Graff-Radford, 2007). Referred pain is often a result of myofascial restrictions or adhesions in soft tissue, causing sensation in areas other than the primary site. It has been shown that “myofascial pain is a common symptom of TMD –it is often associated with the clenching of teeth, grinding and stress” (Wieckiewicz, Beoning, Wiland, Shiau, & Paradowska-Stolarz, 2015).
 In addition to manipulation of soft tissues of the neck, face, and scalp, massage therapists often address TMD directly by treating intra-orally, (inside the mouth), which allows access to tissues that cannot be effectively reached on the surface of the face or head. This type of specific treatment can help improve the level of pain and dysfunction experienced with TMD. A study testing this course of action included a series of intra-oral techniques performed by a chiropractor, and tested pain levels and mouth opening range of motion. The results of this randomized controlled trial (RCT) showed “statistically significant differences in resting, opening and clenching pain, opening scores, and global reporting of change” (Kalamir, Bonello, Graham, Vitiello, & Pollard, 2012). Improvements measured were gained over 10 treatment sessions within 5 weeks, and lasted for up to one year.
In addition to manipulation of soft tissues of the neck, face, and scalp, massage therapists often address TMD directly by treating intra-orally, (inside the mouth), which allows access to tissues that cannot be effectively reached on the surface of the face or head. This type of specific treatment can help improve the level of pain and dysfunction experienced with TMD. A study testing this course of action included a series of intra-oral techniques performed by a chiropractor, and tested pain levels and mouth opening range of motion. The results of this randomized controlled trial (RCT) showed “statistically significant differences in resting, opening and clenching pain, opening scores, and global reporting of change” (Kalamir, Bonello, Graham, Vitiello, & Pollard, 2012). Improvements measured were gained over 10 treatment sessions within 5 weeks, and lasted for up to one year.
Although there has not been extensive research conducted concerning the use of massage therapy in the treatment of jaw pain and dysfunction, there are some studies that show positive results. A literature review to determine the efficacy of manual therapy for TMDs determined that, “the few quality RCTs on manual therapy for TMD indicate that it is a viable, cost effective and reversible mode of conservative treatment” (Kalamir, Pollard, Vitiello, & Bonello, 2007). An article that identifies massage therapy as a choice conservative treatment option for individuals experiencing TMD states that symptoms can be relieved, but also reported that patients require “at least 8 therapeutic sessions to receive true relief” (Wieckiewicz, Beoning, Wiland, Shiau, & Paradowska-Stolarz, 2015). This point, along with the data recorded in the above-mentioned intra-oral RCT, supports what many therapists and clients know from experience – a series of treatments, in association with practiced client “homework,” is often necessary to affect lasting changes.
Alicia Harvey-Stoffberg, RMT, BHS
References
Graff-Radford, S. B. (2007). Temporomandibular disorders and other causes of facial pain. Current Pain and Headache Reports , 11, 75-81.
Kalamir, A., Bonello, R., Graham, P., Vitiello, A. L., & Pollard, H. (2012). Intraoral myofascial therapy for chronic myogenous temporomandibular disorder: a randomized controlled trial. Journal of Manipulative and Physiological Therapeutics , 35 (1), 26-37.
Kalamir, A., Pollard, H., Vitiello, A. L., & Bonello, R. (2007). Manual therapy for temporomandibular disorders: a review of the literature. Journal of Bodywork and Movement Therapies , 11 (1), 84-90.
Wieckiewicz, M., Beoning, K., Wiland, P., Shiau, Y., & Paradowska-Stolarz, A. (2015). Reported concepts for the treatment modalities and pain management of temporomandibular disorders. The Journal of Headache and Pain , 16 (106).
